Effects of botulinum toxin type A in a migraine-specific animal model
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 28 April 2025
Authors
Background: OnabotulinumtoxinA (BoNT/A) is an established treatment for chronic migraine, although the detailed molecular mechanisms underlying its efficacy remain unclear. In this study, we examined the anti-hyperalgesic effects of BoNT/A using an animal model of migraine induced by nitroglycerin (NTG) administration associated with the orofacial formalin test, aiming to enhance our understanding of the modulatory effect of the drug on migraine pain pathways.
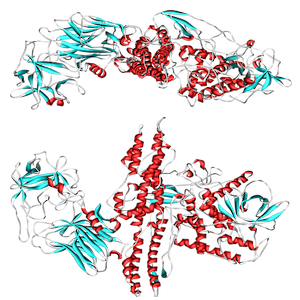
Methods: Male rats weighing 235-240 g (n=7 per group) were used. BoNT/A (10 U/kg) was administered unilaterally as a 25 μL bolus into the right upper lip. Rats in the control group received an injection of 25 μL of 0.9% saline. Seven days after BoNT/A injection, rats were administered NTG (10 mg/kg, i.p.) or its vehicle and were subjected to the orofacial formalin test 4 hours later. At the end of the behavioral test, the medulla-pons area and the trigeminal ganglia were collected and processed for RT-PCR analysis.
Results: At the orofacial formalin test, the NTG-treated rats had a more marked nocifensive behavior compared to vehicle-treated animals. BoNT/A pretreatment significantly reduced this behavior. In addition, calcitonin gene-related peptide (CGRP), pituitary adenylate cyclase-activating peptide (PACAP), and vasoactive intestinal peptide (VIP) mRNA levels were higher in the NTG-treated group in trigeminal ganglia on both sides compared to the control group, with CGRP and PACAP mRNA levels being higher on the side ipsilateral to BoNT/A injection. BoNT/A pretreatment in NTG animals reduced CGRP and VIP gene expression on both sides, while PACAP gene expression was reduced only on the trigeminal ganglion (TG) ipsilateral to BoNT/A injection. NTG treatment induced an increase in mRNA levels of all neuropeptides in the medulla-pons region, which was attenuated by BoNT/A pretreatment.
Conclusions: A single BoNT/A pretreatment attenuated mRNA upregulation of sensory neuropeptides induced by the NTG challenge in the trigeminal ganglia and medulla-pons regions.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






